“Sticks and stones may break my bones, but words will never harm me.”
We all know from experience that the old idiom isn’t true. But what about when it comes to language used in patients’ medical records? Do we need to be extra cautious about the terminology and patient descriptors being used? Can language impact quality of care?
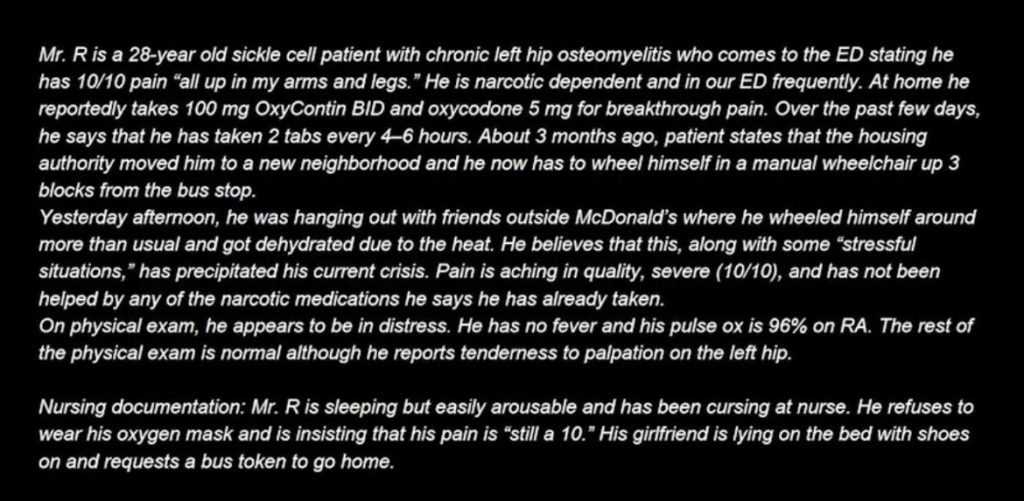
One excellent study performed by Goddu et al in 2018 presented emergency medicine and internal medicine trainees with two different versions of a medical record note. The patient was the same for both versions: an individual with sickle cell disease who needed treatment for pain. All clinically relevant information was the same, but one version had stigmatizing language planted in it, and the other had neutral language.
Check out the stigmatizing version pictured at the bottom of this post. What parts can you identify as being stereotyping or stigmatizing?
Here are a few:
· “all up in my arms and legs”
· Narcotic dependent
· In our ED frequently
· Housing authority moved him to a new neighborhood
· Hanging out with friends outside McDonald’s
· He refuses to wear his oxygen mask and is insisting that his pain is “still a 10”
At first glance, some of these statements might seem harmless. Yet each one falls into one of three categories that give subtle, unhelpful (at best) messages about the patient:
1. Casting doubt on the patient’s pain (e.g. insisting that his pain is “still a 10” vs. still has 10/10 pain).
2. Implying patient responsibility with references to uncooperativeness (e.g. he refuses his oxygen mask vs. he is not tolerating the oxygen mask).
3. Portraying the patient negatively (irrelevant and unnecessary indicators of socioeconomic status are used, such as the reference to housing authority and McDonald’s).
Goddu’s study found that trainees’ exposure to the stigmatizing language was associated with:
· More negative attitudes towards the patient (20.6 stigmatizing vs. 25.6 neutral. P < 0.001)
· Less aggressive management of the patient’s pain (5.56 stigmatizing vs. 6.22 neutral. P – 0.003).
Interestingly, the trainees could also identify the planted, stigmatizing language following the study.
Goddu concluded that stigmatizing language used in medical records to describe patients can influence subsequent physicians-in-training in terms of their attitudes towards the patient and their medication prescribing behavior.
Have you encountered EHR documentation that is stigmatizing? Have you noticed an impact on the patient’s care?
Source: https://lnkd.in/gUBjYgPC
